1 United Healthcare denies claims of a coma patient, says doctor in a viral post
1 UnitedHealthcare Denies Coma Patient’s Claims: Doctor’s Viral Post Sparks Outrage

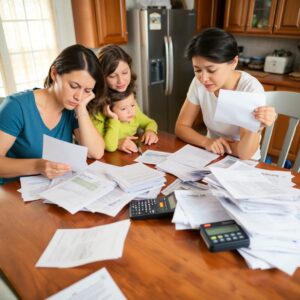
A recent viral social media post has ignited significant outrage regarding UnitedHealthcare’s decision to deny claims for a coma patient. In the post, a concerned doctor shared an image that depicted the heartbreaking situation of a patient who has been in a coma for several months. The doctor claimed that despite the urgency and necessity of the medical services, the insurance company rejected the patient’s claims, leaving the family in a dire situation. This emotional plea resonated with many, igniting discussions about the crisis in healthcare claim denials.
UnitedHealthcare, a prominent player in the healthcare insurance market, has faced increasing scrutiny over claim denials. As more patients find themselves battling insurance companies to receive necessary medical treatments, concerns over claims processing and decision-making grow. This article will investigate this specific case, explore reasons behind the denial, analyze broader implications for patients and the healthcare system, and provide actionable steps for navigating similar situations.
The Case Details: UnitedHealthcare’s Denial

The Patient’s Condition
The patient in question has been in a deep coma for over six months after a severe traumatic brain injury (TBI). TBIs can cause lasting damage, requiring extensive medical interventions. The patient’s treatment involved several costly procedures, including:
- Intensive care unit (ICU) stays
- Neurological evaluations
- Rehabilitation therapies
This situation underscores the complexities surrounding critical care and the necessity for insurance coverage in such life-altering circumstances.
The Claim
The denied claim included a total of $500,000 for various treatments. This amount often includes hospital stays, surgeries, and rehabilitation services essential for recovery. The rejection of such a significant claim can place immense financial strain on a family already grappling with the uncertainty of a loved one’s health.
UnitedHealthcare’s Response
UnitedHealthcare has issued a statement regarding the denial, highlighting the need for appropriate documentation and pre-authorization for certain treatments. Their response has done little to quell the anger and frustration felt by many, as families continue to struggle with navigating insurance policies that seem to place obstacles in the path to necessary medical care.
Reasons for Claim Denial: Exploring the Possibilities

Pre-authorization Issues
Pre-authorization is a critical step for many medical services. When not obtained, it can lead to significant claim denials. Statistics show that nearly 25% of pre-authorization requests are denied by insurance companies. This can leave patients and families in a bind, as they may feel forced to make healthcare decisions without complete knowledge of potential coverage.
Policy Exclusions
Insurance policies may contain exclusions that could justify the denial. Common examples include:
- Pre-existing conditions
- Treatments deemed experimental
- Non-covered services
Understanding these exclusions is vital for patients to recognize potential pitfalls when filing claims.
Documentation Gaps
Proper documentation is crucial in supporting medical claims. Incomplete or missing paperwork can lead to quick denials, forcing families to navigate a complex appeals process. Ensuring all medical records and treatment plans are comprehensive can make a significant difference.
The Broader Implications: Healthcare System Challenges
Patient Advocacy
Patient advocacy groups play a critical role in helping families challenge insurance denials. Organizations like the Patient Advocate Foundation and Families USA can provide resources and support for those facing similar issues. Effective advocacy can often lead to a successful re-evaluation of denied claims.
Healthcare Costs
Rising healthcare costs have become a massive concern for many families. Over 40% of Americans report feeling anxious about medical bills, with many facing significant medical debt. The combination of high costs and insurance denials puts patients in precarious situations.
Insurance Industry Practices
Systemic issues within the insurance industry contribute to the challenges faced by patients. Profit-driven incentives often motivate insurers to deny claims, leading to increased scrutiny of their practices and policies. Addressing these issues may require comprehensive reforms within the industry.
Navigating Insurance Claim Denials: Practical Advice
Understanding Your Policy
Patients must thoroughly review their health insurance policies to identify coverage limits and exclusions. Knowing what is covered can save significant stress when it comes to filing claims.
Appeals Process
If a claim is denied, patients should follow a clear appeals process:
- Review the denial letter for specific reasons.
- Gather necessary documentation, including medical records and bills.
- Submit a formal appeal within the designated timeframe.
- Follow up regularly to check on the status of the appeal.
Successful appeals often involve thorough documentation and clear communication.
Seeking Legal Advice
In certain cases, it may be necessary to seek legal counsel. Insurance disputes can be complex, and medical malpractice lawyers often have the expertise to guide families through the legal landscape surrounding their claims.
Conclusion: Lessons Learned and Call to Action
The outrage over the denial of a coma patient’s claims highlights significant issues within the healthcare system. The case illustrates how pre-authorization challenges, policy exclusions, and documentation gaps contribute to a larger problem faced by many.
Readers are encouraged to advocate for changes within the healthcare system. Sharing experiences and demanding transparency from insurance companies can be powerful tools for change. As public awareness grows, we may see shifts in healthcare policies that support patients rather than hinder them. The impact of this case may resonate in future healthcare debates, influencing both policy and public perception of insurance practices.














1 comment